Acute Pancreatitis in pregnancy

Abstract
Introduction
Acute pancreatitis is an inflammatory condition of the pancreas characterized clinically by abdominal pain and elevated levels of pancreatic enzymes in the blood. The pathogenesis of acute pancreatitis is not fully understood. Nevertheless, a number of conditions are known to induce this disorder with varying degrees of certainty.
Methods/Methodology
We present the case of a patient who had an episode of acute biliary pancreatitis at 36 gestational weeks.
Conclusions
Acute pancreatitis during pregnancy remains a difficult clinical problem to manage.
Introduction
The pathogenesis of acute pancreatitis is not fully understood, but a number of conditions are known to induce this disorder, with gallstones and chronic alcohol abuse accounting for two-thirds or more cases in the United States [1].
Acute pancreatitis is rare during pregnancy. In a retrospective cohort study of 16,000 deliveries, only eight cases of acute pancreatitis were noted; five were due to gallstones and the others were idiopathic [2].
A number of cases of hyperlipidemia associated with pancreatitis in pregnancy have also been reported. Hyperlipidemic gestational pancreatitis usually occurs only in women with preexisting abnormalities of lipid metabolism, although it is not clear if pregnancy increases the risk of pancreatitis in women who have underlying hypertriglyceridemia.
Patients who developed pancreatitis in the first trimester of pregnancy had the highest risk of fetal loss (20%) and pre-term delivery (16%).
Acute pancreatitis is a rare event during pregnancy which occurs in about 3 out of 10,000 pregnancies. The most common causes of acute pancreatitis in pregnancy are: gallstones and hypertriglyceridemia. First line treatment is conservative, but the relapse rate is 70%; acute biliary pancreatitis during pregnancy is associated with a significant maternal and fetal mortality rate. The maternal and fetal mortality rate is 20% and 50% respectively [3].
There are no reports concerning the teratogenicity of the treatment, described for other drugs [4] or not [5] – same as for molar pregnancy [6] – or the influence on the possible cellular mechanism [7], [8], [9] or innervation [10] of the uterine muscle with risk of premature delivery. Preeclampsia [11] or infertility treatments [12], with their side effects [13], [14], [15], seem, neither, related to this pathology.
Case report
A 31-year-old (so, no amniocentesis [16] was needed), primigesta, primipara pregnant woman, at 36 weeks presents to the emergency service for epigastric pain with irradiation in the right and left hypochondrium. Following clinical, paraclinical and interdisciplinary examinations the patient was diagnosed with acute pancreatitis, caused by gallbladder problems.
Paraclinical Exams
We noted the serum amylase value which was 30 times higher than the normal one (3163 UI/ L), undetectable lipase, and the rest of the blood tests within normal range.
Abdominal ultrasound revealed gallstones with diameters between 3 and 8 mm, and a partially visible pancreas.
Our diagnostic was lithiasic pancreatitis.
An interdisciplinary commission was formed, consisting of a surgeon, a gastroenterologist, an obstetrician who decided having an urgent cesarean delivery (so, no adapted partogram [17] was possible in this case), with a usual spinal anesthesia, without having the time to reflect on alternative possible drugs for this [18]. We extracted a live, normal, fetus, single female sex, weight 3180g, Apgar 9 and transferred the patient to the intensive care department.
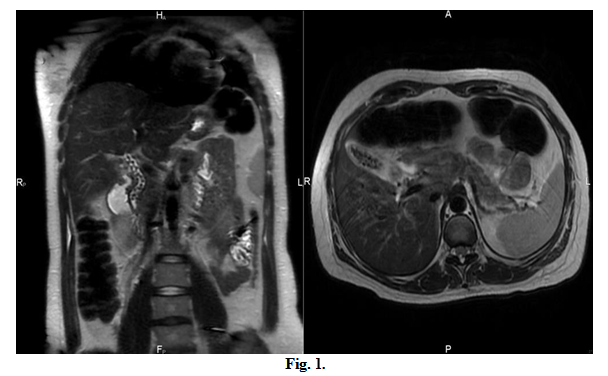
Following the colangio-IRM (Fig. 1), the gastroenterologist recommended delaying the ERCP (Endoscopic Retrograde Cholangiopancreatography) by 7 days, after surgery a. Also, he opted for a cholecystectomy after the termination of the confined period
Further favorable evolution was noted, after having the ERCP done, with normalization of pancreatic values.
Discussion
The patient was HIV-negative, so no immunological suppression was observed [19], without any other pre-gestational pathologies, difficult to assess etiologically [20], [21], [22], or other pain-inducing pathologies [23], [24].
It seems that pregnancy increases the risk biliary pathology [25] – which could be related to a pancreatic pathology, but in this patient, it was not the case.
Conclusion
Acute pancreatitis during pregnancy remains a difficult clinical problem to manage.
IZVORANU Silvia [1]
PENCIU Roxana [1]
STERIU Liliana [1]
MOCANU Diana [1]
NICULESCU Costin [1]
POSTOLACHE Iulia [1]
[1] Obstetrics-Gynaecology Clinic I, Saint Andrew Clinical Emergency Hospital Constanta, (ROMANIA).
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “SOGR 2018 – 17th National Congress of the Romanian Society of Obstetrics and Gynecology & First Advanced Colposcopy Course - 2018”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “SOGR 2018 – 17th National Congress of the Romanian Society of Obstetrics and Gynecology & First Advanced Colposcopy Course - 2018”
To buy the Proceedings click here.



