Aging at the interface of biology and culture

Abstract
The number of persons aged 65 and older is increasing dramatically worldwide, with a worrisome rising burden of disease, and a strong public health concern. Biomedical research of aging is continuously providing major knowledge in terms of molecular, cellular, genetic, and clinical findings, but the nature of aging differs across older populations and worldwide. So far, frontline research follows a reductionist paradigm where major domains of culture and biology remain separated. Moreover, the field of Gerontology has been limited by focusing primarily on developed countries, in terms of basic, translational, and clinical research. Indeed, the current discussion on normal aging gives the impression that there is one way to age. Instead, evidences show that aging is under the influence of dynamic multidirectional factors, which also include behavior, choice, chance, culture, and environment with epigenetic factors. All such factors are able to influence the type and quality of aging, and health and become a matter for anthropological approaches. In this arena, biology and culture meet and we learn that healthy behaviors and environments are essential factors of healthy aging, and reduce vulnerability during elderly. By contrast, unhealthy environments – amenable to primary prevention measures – increase the gap in ability between elderly and young people. This scenario anticipates enormous sanitary and economic consequences.
Acknowledgements
The following colleagues contributed to constructive discussions over the years: Giuseppe Palasciano, Peter Malfertheiner, Tom LaMont, Hermon Dowling, Gerard vanBerge Henegouwen, Monica Acalovschi, Dan L. Dumitrascu, Paolo Livrea, Francesco Di Benedetta, Francesco Vitiello†, Giuseppe Baldassarre, Agostino Di Ciaula, Marina Nuzzo, Emilio Molina-Molina, Harshita Shanmugam.
Table of Contents:
1. The aging population
2. Factors Involved in the Aging Process
3. Anthropological Aspects
4. Aging: a Holistic Perspective
5. Conclusions
1. The aging population
The number of persons aged 65 and older is on the rise. In addition, the speed of population aging is rapidly increasing worldwide according to the World Health Organization (WHO) [1]. In
2016 in US the number of people aged ≥65 were 42.2 million, 58% were aged 65-74, 29% were aged 75-84, and 13% 85 and older [2]. Worldwide, the number of adults over 60 years of age will exceed 20% by 2030 or over 70 million people [3], and 2 billion by 2050, representing over 20% of the world’s population [4]. Also by 2050, 80% of older people will be living in low- and middle- income countries [1]. While about 20% of the population of the developed world is currently over 60 years of age, analyses predict that about 30% of the population will be over 60 years old by 2030 in developed countries [5], due to the increase in life expectancy plus trends of historical fertility.
Notably, developing countries display a lower life expectancy, with a percentage of older adults relatively low. By contrast, in the developed world, the number of individuals aged ≥60 yrs. is greater and this population is growing faster than populations in the developed world [5]. As an example, in Japan, the population over 65 has doubled from 7% to 14% in 26 years. The trend is similar in other Asian countries, pointing to a very rapid change of the population. As comparison, similar changes occurred in the last century in Europe [5].
This trend is true in both developed and developing countries and is associated with public health concern. Health and well-being of elders will absorb huge socio-economic resources.
Analyses at our internal medicine division in a large academic hospital in southern Italy indicate that both hospitals stay and hospital costs increase with age (M Nuzzo and P Portincasa, Presentation at the Congress of the Italian Society of Internal Medicine – SIMI – Rome, 2018).
2. Factors Involved in the Aging Process
Understanding aging is one of the most complex issues now facing contemporary Science. One basic question is when does late life begins. Current view considers the “young-old” (65-79 years), the “old-old” (80-99 years), and the “oldest old” (i.e., 100 or more years, centenarians).
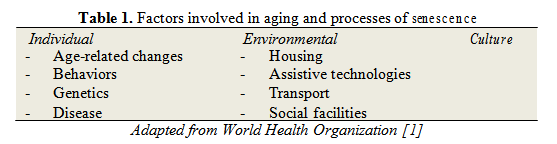
Age refers to the number of years a person has been alive. The term cohort refers to a group of people who share the same birth year or sometimes those who shared historical events. A cohort is the one as the World War II generation. The word period refers to the time at which the assessment occurred. The age effect occurs if a particular phenomenon always changes with age, irrespective of cohort or period. The cohort effect occurs if the change is specific to a particular cohort but does not occur in any other group. A period effect occurs if all cohorts or ages change at a particular point in time. Older adults represent a great proportion of the population across all cultures. Several aspects, however, are different in senescent people in terms of environmental influences, biology, and behavior. Major factors involved in aging and processes of senescence appear in Table 1.
Every older person is indeed different, as indicated by WHO. Some older persons will function like a 30-year-old person, while many old persons will fail this task and require full time assistance [1]. According to the current view, age would represent not a cause of effects, but rather an index to the accumulating effects of many causes [6].
3. Anthropological Aspects
Aspects of aging have been the object of study by biological anthropologists. Matter of discussion include the essence of chronic disease, bone and reproductive biology, and body composition over the scenario of demographics, which is rapidly changing [7].
An essential aspect to consider is the increase in life expectancy during the hominid evolution. One striking aspect in evolutionary biology is that the estimated maximum lifespan has almost doubled. The difference is enormous, i.e., from our ancestors Australopithecines with approximately 53 years (and 15 year life expectancy) to modern humans with about 122 years (and now 83 year life expectancy) [8-11]. This enormous gap in life expectancy has occurred in the last 200 years [9]. In the United States, a similar increasing trend has occurred in less than 100 years, i.e., life expectancy has increased from 46 years (in 1900) to 77 years (in 1997) [12, 13]. In spite of a general trend in increase of life expectancy worldwide, differences are still striking across populations. Observations show that life expectancy is as low as 35 years in Botswana but raises to 83 years in Andorra [2]. Thus, the research is now focusing on the question if the increase in human life expectancy will continue to occur in the world [14, 15]. Some pragmatic aspects exist in this respect. Epidemics might drastically affect these trends. HIV/AIDS in Africa contribute to decrease life expectancy in that continent, and this aspect increases the gap between developing and developed countries [16].
4. Aging: a Holistic Perspective
The results of such rapid changes in aging imply that societies, health systems, individuals and government must adapt to the new scenarios. An anthropological perspective is welcome in this context, since a biomedical research follows rather reductionist hypotheses. Biomedical research indeed tends to separate the biology from the cultural domains, and recapitulates straight unidirectional perspectives and directions [17], instead of looking at the rather multidirectional influence of several factor. These factors include behavior, environment, culture, which all will affect health.
Studies conducted in the scientific context of Gerontology depict a rather “normal” aging, i.e., within the Baltimore Longitudinal Study of Aging (BLSA) [18]. The scientists explored age- associated changes in anatomical integrity and function across all physiological systems, including musculoskeletal, cardiovascular, endocrine, renal, etc.). This study concludes that genetic factors influence aging and longevity. However, apparently simple environmental factors also greatly influence the quality of our own aging, and include watching a person’s weight and waist, eating a healthy diet, exercising regularly, refraining from tobacco use, and maintaining an active role in the society. At variance with genetic factors, almost all environmental, cultural and socio- economic factors influencing healthy aging are modifiable, leading to possible actions (public- health oriented policies) aimed to primary prevention.
Environment and epigenetic factors
Environmental factors do modulate vulnerability during elderly. A healthy environment contributes to extra years passed in good health, a condition when there is little difference in ability level, as compared with young people. Conditions in older age are non-communicable diseases, and healthy environment and behaviors contribute to reducing the risk of non-communicable diseases and improving physical and mental capacity. By contrast, the unhealthy environment contributes to fast decline in both physical and mental capacity, with the ultimate result of negative implications for older people and for the society.
Another aspect is that environmental factors can influence the aging process at an early stage. In particular, the environments that people live in as children, or even as developing foetuses, together with their personal characteristics will produce long-term effects on how they age. The role of epigenetic factors is essential, and the pathway includes the environment continuously interacting with body cells and the epigenome (i.e., histone modification, DNA methylation, miRNA mediated gene silencing, evolution of inherited genome, and gene polymorphism, ultimately leading to disease onset if the system becomes unbalanced. Wang et al., [19], investigated the Great China famine exposure during infancy. Exposure in 2,148 participants was associated with increased risk of metabolic syndrome (P=0.004) in adults aged 50s and occurring in the three exposed groups, i.e., foetal, infant, and preschool. The study provided further evidence for the developmental origin’s hypothesis. In the Dutch famine studies [20, 21], the authors measured body size of 741 people born at term between 1943 and 1947 in Amsterdam.
They compared people exposed to famine in late, mid, or early gestation with non-exposed people born before or conceived after the famine period. The study found that maternal malnutrition during early gestation was associated with higher body size and waist circumference in 50-y-old women but not in men. Again, perturbations of central endocrine regulatory systems during in early gestation may contribute to the development of abdominal obesity in later life. Notably, the major difference between exposed and non-exposed same-sex siblings in the Dutch famine study was the presence of different DNA methylation patterns. These findings underlie the role of epigenetic factors in the onset of obesity in later age [22]. In another recent study relating DNA methylation with healthy aging of elderly twins [23], the authors identified similar epigenetic mechanism. The research examined frailty index as a quantitative indicator of biological age, and quantitative DNA methylation data on genome-wide CpG sites. The study suggests that DNA methylation at CpG sites in the promoter region of PCDHGA3, is a key mediator of healthy aging, and is associated with biological age.
The WHO calculates 250,000 possible deaths/year between 2030 and 2050 caused by the negative effects of climate change. Aged subjects are particularly vulnerable to direct health effects of climate change, mainly in terms of heat-related mortality. A recent Chinese study estimated a 264% (117.5% to 427.3%) increase of heat-related mortality in the 2080s as compared with the 1980s in the absence of effective mitigation measures. [24]. Projections are worrisome and should call for preventive policies. Di Ciaula conducted a study in elderly people (>70 yrs.), and reported a correlation between number of emergency visits and daily air concentrations of particulate matter of less than 10um (PM10), and of nitrogen dioxide (NO2) measured at 1 and 3 km from a gas-fired power plant. The conclusions were that short- and long-term exposure to air pollutants would have major health consequences. A striking effect occurs in terms of cardio- respiratory diseases, and is more evident in vulnerable aged people [25]. A Korean study examined 502 subjects aged 60 yrs. or more, and demonstrated a direct relationship between polycyclic aromatic hydrocarbons (PAHs) exposure and insulin resistance [26]. The authors underscored the role of an unhealthy environment in generating a number of metabolic effects. Another study evaluated the interaction of particulate air pollutants on APOE alleles, as potential contributors to Alzheimer’s disease. The authors studied the neurodegenerative effects of particulate air pollutants in a US-wide cohort of older women from the Women’s Health Initiative Memory Study (WHIMS), as well as in experimental mouse models. Particulate matter exposure over the EPA standards promotes pathological brain aging in older women. Effects include increased risks for global cognitive decline (+81%), and all-cause dementia (+92%), with a stronger adverse effect in APOE ε4/4 carriers. The underlying mechanisms may involve increased cerebral Abeta production and selective changes in hippocampal CA1 neurons and glutamate receptor subunits [27]
Diet
As the age passes, eating well-balanced diet becomes important [28]. Proper instruction for a healthy diet contributes to lower the risk of developing chronic health conditions. The optimal body mass index (BMI) in the older adult is higher than BMI for younger adults. BMI should range 24 to 29 kg/m2 [29]. Subjects should eat small amounts but frequently, healthy diet, with supplementation with vitamin B12 [30], and vitamin D [31]. Calcium supplementation to 1,200 mg/day is also recommended [31], because the intestinal absorption of calcium decreases after the age of 60, and to prevent osteoporosis and fractures [32]. Up to 70% of older patients carry a nutritional risk or display malnutrition [33]. As malnutrition is associated with increased mortality risk [34], a screening for nutritional status is required in older patients [35]. A clinically significant weight loss must be prevented (i.e., at least 5% of body weight over a period of 6 to 12 months).
In patients with weight loss and frailty, several detrimental factors must be carefully ruled out by appropriate screening questionnaires, including medications, depression, social factors, psychologic factors, chewing and swallowing problems, eating dependency and unnecessary dietary restrictions (low-salt/low-fat) [36]. Treatment of weight loss is essential in older patients, trying to restore the baseline weight, and using specific algorithms for estimation of energy requirement. Nutritional supplementation and appetite stimulants might be required.
Physical activity
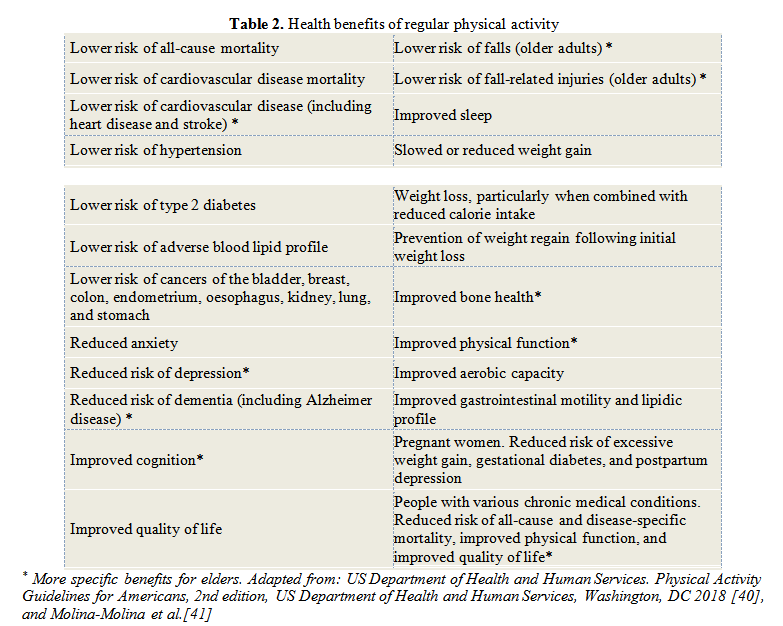
Constant physical activity, especially by resistance training (RT), also promotes healthy aging. At a muscle gene and protein expression, the regulation occurs at multiple levels, influencing both baseline phenotype and responsiveness to a resistance training. Molecular networks include genome, DNA modification and methylation, transcriptome, alternative splicing and post- transcriptional regulation with production of miRNAs, muscle protein synthesis with influence on the proteome [37]. Neuromuscular benefits include adaptations seen in the skeletal muscle after the force generated during muscular contractions, augmented force production, power and overall strength, increased mobility as well as better balance [37]. Regular physical exercise anticipates a series of additional benefits specific to the elders. Gains include lower risk of cardiovascular disease (including heart disease and stroke), improved cognition, reduced risk of dementia (including Alzheimer disease), reduced risk of depression, improved bone health, physical function, lower risk of falls and of fall-related injuries (older adults). Appropriate counselling is a must for older adults [38, 39]. For people with various chronic medical conditions, moreover, benefits include reduced risk of all-cause and disease-specific mortality, improved physical function, and improved quality of life (Table 2) [40].
Art therapy
Aging is associated with rising prevalence of dementia, and effective pharmacological treatments are missing. Psychosocial interventions might alleviate the effects of dementia and influence the quality of life, as well. In this context, there are growing evidences showing that visual art, music and dance might be beneficial through direct and indirect effects, and with minimal costs. For example, coloring pictures and art therapy have positive effects on mood, alleviating depression and apathy in dementia. This approach is part of a more consensus, asking for more cultural, and social inclusion of people with dementia, including elders [42].
In a recent systematic review and meta-analysis, the authors examined the impact of musical practice on healthy neurocognitive aging [43]. Based on 13 selected studies, the authors confirmed cognitive and cerebral benefits of musical practice, both in domain-specific functions (auditory perception) and in other rather domain-general functions. Notably, these benefits appear to protect cognitive domains that usually decline with aging and boost other domains that do not decline with aging.
One way to aging?
As underscored by the WHO, healthy ageing is “…being able to do things we value for as long as possible”. Options include a change in the way we think about ageing and older people, creation of age-friendly environments, alignment of health systems to the needs of older people, and development of systems for long-term care [1].
According to the new BLSA paradigm of functional aging, “mobility” is the key outcome measure. The hierarchical model evolves from the left block which includes the essential homeostatic/behavioral elements (i.e., hormones, inflammation, immune function, sleep and rest, nutrition and engagement), to the central physiological domains which are relevant for mobility.
Sub-elements in this block include the role of the central nervous system in accord with the peripheral nervous system. Muscles are effectors moving bones and joints, while the mobility requires energy generated, transported, and delivered locally. The somatosensory systems provide continuous feedback from the environment. According to the paradigm, the mobility problems in older persons originate from multiple, alterations of physiological domains, rather than a single precipitating cause [44]. However, the BLSA was targeted in developed countries and on certain populations within countries, i.e., the majority of individuals. The conclusions drawn from this study indicated that the only logical way to age is the pattern observed with the European-derived individuals. Any other possibility could be a deviant pattern from “normality”. In this scenario, investigators can address only limited questions, and can miss additional aspects, which include economic, evolutionary, environmental, historical, socio-cultural, social connections, and additional complex factors during the process of ageing. Chance and choice also affect how we age [7]. This approach should appear in Gerontology, because it will combine the interplay of several factors operating in a “real life” context. The increasing knowledge about aging is therefore the result of growing knowledge, which include interdisciplinary endeavors, and the aging process.
On another side, the field of bio-gerontology has been expanding when studying aspects related to genetic and cellular mechanisms of aging. Additional knowledge comes from disciplines like psychology, sociology, and anthropology. All such aspects bring a continuous flow of information about the interplay among mental, cognitive, physical health, and sociocultural processes. A consequence related to such a growing field, is the chance for increasing confusion, due to growing research, several theories, different specific biological aspects, findings dependent on time, and populations, as well as deepening of specialties. As a matter of fact, the field of Gerontology is still missing a unifying hypothesis.
A modern view of optimal aging should therefore consider that there are different ways of aging well, different configurations of vulnerabilities, different resources that affect how humans age.
In other words, aging is a process that continually unfolds. The concept of functional health recapitulates the ability to perform daily tasks such as activities of daily life (ADL) and caring for oneself, such as bathing, dressing, and eating. By contrast, instrumental activities of daily living (IADL) include shopping, paying bills, preparing meals, or getting around. Another key aspect is the so-called failure to thrive (FTT) in elderly adults, i.e., a syndrome of global decline that occurs in elders, and which is at the crossroad of physical frailty [44, 45] (malnutrition, weight loss, and poor physical function), impaired neuropsychiatric function (i.e., cognitive impairment and depression), and functional disability (i.e., loss of >1 ADL). External, but still essential modulatory factors include the effects or interactions of medications, comorbidities (i.e., diabetes, tumors, arthritis, congestive heart failure and chronic obstructive pulmonary disease), and psychological factors (i.e., isolation, grief, welfare, abuse and neglect).
5. Conclusions
The current concept of healthy aging must take into account physical, social aspects on a biological and cultural level. Environmental exposures throughout life interact with epigenetic factors. Healthy behaviors and environments are essential components of healthy aging and reduced vulnerability in ageing. By contrast, unhealthy environments increase frailty and the gap in ability between elderly and young people. This scenario anticipates enormous sanitary and economic consequences, and policies should focus on preventive measures to promote healthy environments and a multidisciplinary approach to health in elderly people.
The Authors:
PORTINCASA Piero, MD, PhD, Internist [1][2][3][4][5]
[1] Head, Clinica Medica “A. Murri”, Hospital Policlinico, Bari, (ITALY).
[2] Director, Residency Programme in Geriatric Medicine; Department of Biomedical Sciences & Human Oncology, University of Bari Medical School, Bari, (ITALY).
[3] Member of the Apulian Academy of Sciences.
[4] dr. Honoris Causa, University of Medicine and Pharmacy of Bucharest, University of Medicine and Pharmacy of Cluj-Napoca, University of Medicine, Pharmacology, Science and Technology of Targu-Mures, (ROMANIA).
[5] President-elect Trustee of the European Society for Clinical Investigation (ESCI).
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “Central European Gastroenterology Meeting (CEURGEM) - 2019”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “Central European Gastroenterology Meeting (CEURGEM) - 2019”
To buy the Proceedings click here.



