HIV Infection in Pregnancy

Abstract
Many HIV (Human Immunodeficiency Virus) positive women are of fertile age. The efficiency of antiretroviral treatment determined an increase in HIV positive pregnant women’s prevalence.
Objectives
We evaluated HIV positive pregnant women under HAART (Highly Active Antiretroviral Therapy), trying to determine if the congenital anomaly rate is higher than in normal pregnant population, due to the antiretroviral treatment. Also, we have tried to determine if prenatal screening for fetal anomalies and Doppler evaluation of uterine arteries are influenced by the HIV infection or/and by antiretroviral treatment, HIV pregnancies often being complicated with IUGR (Intrauterine Growth Restriction) or SGA (Small for Gestational Age).
Methods
Our prospective study extended between January 2013 and December 2017. We have evaluated 40 HIV positive pregnant women under HAART therapy. Ultrasound examinations were performed monthly in the first two trimesters and on two weeks interval until birth (first and second trimester screening for fetal anomalies and at least 3 ultrasound examinations after 24 weeks of gestation were compulsory for the admission in this study).
Results
We identified only one case with fetal anomalies, a patient with high risk of Down syndrome determined in first trimester screening for aneuploidy. If there were no complications the pregnancies were terminated by C-section at 38 weeks of gestation. 80% of the births were at term, 20% of the patients had premature labor. From those that gave birth at 38 weeks of gestation, 20% had newborns that weighted over 3000 g, 60% under 3000 g. We mention one case where the pregnancy had to be evacuated prematurely due to maternal conditions (cerebral tumor).
Conclusions
Our study didn’t reveal any association between antiretroviral treatment and fetal anomalies. Uterine artery Doppler evaluation was useful in determining the cases with high risk of developing IUGR, known to have a high incidence in HIV positive pregnancies. We have noticed a higher percentage of premature births in patients with fewer ultrasound and obstetrical examinations.
Table of Contents:
1. Introduction
2. Methods
3. Results
4. Discussions
5. Conclusions
1. Introduction
HIV (Human immunodeficiency virus) infection is the typical example of an emergent disease with an explosive pandemic evolution. It has a major social and economic influence regarding healthcare costs, taking into consideration the fact that these patients undergo chronic lifelong treatments. In present times, in Romania, HIV infection represents a major problem in terms of public healthcare [1].
HAART therapy (highly active antiretroviral therapy) consists of an association of antiretroviral medication, used together in HIV positive patients. The purpose of this therapy is to lower the viral load until it becomes undetectable and improves immune system dysfunction, preventing opportunistic infections and AIDS associated neoplasia. It consists in an association of two NRTI (Nucleoside Reverse Transcriptase Inhibitor) and a NNRTI (Non- Nucleoside Reverse Transcriptase Inhibitor) or a PI (Protease Inhibitor) [2], [3], [4].
Many HIV positive women are of fertile age. The efficiency of antiretroviral treatment caused an increase in HIV positive pregnant women’s prevalence. HAART therapy might have some side effects. Protease inhibitors was associated in some studies with reduced progesterone levels responsible for IUGR, SGA and risk of abortion; NNRTI being suspected of causing fetal anomalies. An immediate start of the treatment after HIV infection was diagnosed, improves maternal survival, lowers the risk of developing opportunistic infections and also decreases the risk of vertical transmission [2], [3], [4], [5].
There are not many studies regarding HIV positive pregnant women incidence in Romania, the use of first and second trimester markers for aneuploidy or the degree of prediction of IUGR by Doppler evaluation of the uterine arteries in these cases. [5], [6], [7], [8], [9].
The incidence of concomitant hepatitis B infection is high. Suffering from this condition also complicates the evolution of the pregnancy and might influence its outcome, mainly by overstressing the liver, thus elevating the morbidity of these cases. Hepatitis B infection in pregnancy is another major healthcare problem in Romania, the number of studies that tried to obtain the actual incidence and prevalence of the disease among pregnant women, being low [10].
2. Methods
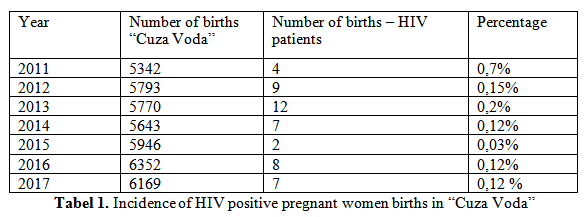
We established the incidence of HIV pregnant women births in our hospital, many of the patients giving birth here because of the close collaboration between obstetricians and infectious disease doctors (Table 1).
We evaluated in our study HIV positive pregnant women under HAART (highly active antiretroviral therapy) therapy, trying to determine if the congenital anomaly rate is higher than in normal pregnant population, due to the antiretroviral treatment. Also, we have tried to determine if prenatal screening for fetal anomalies (first and second trimester fetal morphologic ultrasound scans) and the evaluation of uterine arteries are influenced by the HIV infection or/and by antiretroviral treatment, HIV pregnancies often being complicated with IUGR (intrauterine growth restriction) or SGA (small for gestational age) with a higher morbidity and mortality. Our prospective study extended between January 2013 and December 2017. We have evaluated 40 HIV positive pregnant women under antiretroviral treatment HAART therapy. Ultrasound examinations were performed monthly in the first two trimesters and at two weeks interval until birth. Compulsory for the admission in this study were the first and second trimester screening for fetal anomalies, and at least 3 ultrasound examinations after 24 weeks of gestation. We have excluded from the study all cases with less than 5 ultrasound scans, cases who stopped antiretroviral therapy with no medical indication and those who incorrectly took their treatment throughout pregnancy.
All 40 HIV positive pregnant women had first trimester scan for fetal anomalies and uterine artery Doppler evaluation trying to determine if it can predict the risk for developing IUGR. During ultrasound scan to confirm gestational age first we have measured the fetal crown – rump length (CRL). Then we have measured fetal nuchal translucency thickness (NT), determined the presence/absence of the nasal bone and evaluated tricuspid regurgitation, ductus venosus and the uterine arteries. Between 20 and 24 weeks of gestation all pregnancies had a second scan to evaluate the anatomy of the fetus and also another Doppler evaluation of uterine arteries. At least three more ultrasound scans and the evaluation of the pulsatility indexes of the umbilical artery and middle cerebral artery were needed after 24 weeks of gestation to properly asses and difference IUGR from SGA. If there were no complications the pregnancies were electively terminated by C-section at 38 weeks of gestation to decrease vertical transmission. The pregnancies that developed IUGR or SGA were monitored by periodically determining umbilical and middle cerebral artery Doppler pulsatility indexes and non-stress tests adjusting the period of time to repeat them to the individual evolution of each case. All the data obtained were statistically analyzed using t- student test.
3. Results
From all 40 cases, in only one case we determined fetal anomalies-trisomy 21, a patient with high risk pregnancy for Down syndrome, determined in the first trimester screening for aneuploidy. The patient was informed about this risk, but she refused all other investigations needed to establish if the fetus does or does not have Down syndrome, being determined to keep the pregnancy no matter the outcomes.
In the absence of complications, the pregnancies were terminated by C-section at 38 weeks of gestation. In our case, none of the pregnancies complicated with IUGR or SGA needed evacuation before 38 weeks of gestation due to fetal conditions. Non-stress tests and unaltered Doppler evaluations permitted to continue the pregnancies until 38 weeks of gestations, none of the fetuses with IUGR developing acute distress. 20% of the patients gave birth to newborns that weighted over 3000 g, 60% under 3000 g. The fetal growing curves were evaluated using Astraia software to establish the cases with IUGR and with SGA. From all 40 cases, 25% of the fetuses had IUGR and 25% were SGA, confirming the data from literature that HIV positive pregnancies under antiretroviral treatment often develop these two complications. The presence and the length of the nasal bone were attained during both first trimester and second trimester scans for fetal anomalies. In all pregnancies, except the one that had a trisomy 21 fetus, the length of the fetal nose was in normal parameters according to nomograms. Apgar scores were lower than average for normal uninfected pregnancies due to the delayed adaptation to extra-uterine life. From all cases, 45% of the newborns were admitted to intensive care units with respiratory problems due to delayed adaptation. All of them adapted quickly, being discharged from the intensive care unit in maximum 3 days, with no other complications.
20% of the HIV pregnant women had premature labor, in only one case the pregnancy had to be evacuated due to maternal conditions (cerebral tumor). The discovery of the maternal cerebral tumor led to the evacuation of the pregnancy after corticosteroid administration in order to assure pulmonary maturity, with the intention of saving both the mother and the baby.
We have also observed a high prevalence of hepatitis B infection among our patients, 25% being infected. We didn’t find any statistically significant association between HIV positive patients that also suffer from hepatitis B, and pregnancy evolution, complications or outcomes.
4. Discussions
We have observed a high prevalence of premature labor in all the cases that had less ultrasound scans and obstetrical examinations. Pregnancies with less medical observation tend to develop more complications with untreated vaginal and urinary infections, with no treatment in case of shortening cervix, all of these leading to premature delivery. Less followed HIV positive pregnant women usually have a low socio-economical status, being difficult for them to come more often to the doctor and to have their pregnancies evaluated.
One other cause that leads to less medical surveillance of these women and should be taken into consideration, is the fear of being discriminated, in the present study group of women, all of them stating the fact that they thought at least once about it.
The study group of patients was inhomogeneous regarding the stage of HIV infection, the viral load, CD4 lymphocyte count and the association of antiviral medications in HAART therapy. Because of the low number of cases, only 40 in almost 4 years, it is hard to try and obtain a more homogeneous study population and none of the studies found in the literature had such division of the affected population. The most common associations of antiviral medication in the HAART therapy are: Kaletra (Lopinavir and Ritonavir – protease inhibitors) and Combivir (Lamivudine and Zidovudine-NRTI). The patients with concurrent hepatitis B infection had no medication for it during pregnancy. All cases with newborns over 3000 g had low or undetectable viral loads with A1, A2, B1 or B2 AIDS stages. It becomes clear that such a differentiation between patients should be done, considering the evolution of the pregnancy, the possible complications and outcomes.
We did not find any alterations in the length of the nasal bone, the values of uterine arteries or ductus venosus pulsatility indexes, considering the nomogrames for the gestational age, these ultrasound parameters being unaltered by the disease and/or by the treatment. Delayed adaptation to extra-uterine life and a high number of newborns admitted to intensive care units for short periods of time, appear in these cases because of the evacuation of pregnancies electively at 38 weeks of gestation, many of them with no uterine contractions being present.
5. Conclusions
Our study did not reveal any association between antiretroviral treatment and fetal anomalies. The incidence of fetal anomalies we found was 2.5%, similar to the one found in the unaffected pregnant population, confirming the fact that neither HIV infection, neither antiretroviral treatment has such an effect.
Uterine artery Doppler evaluation was useful in determining the cases with high risk of developing IUGR, with a high incidence in HIV positive pregnancies. All pregnancies that later developed IUGR had notch present in the uterine artery Doppler evaluations, the rest of the patients having normal aspect uterine artery Doppler evaluation and normal pulsatility index. Uterine artery evaluation must be used in the evaluation of these pregnancies to improve the outcome by being able to predict this complication and to adjust medical care in order to decrease mortality and morbidity.
We have observed a high incidence of IUGR and SGA in these pregnancies, confirming the observations found in the literature, that antiretroviral treatment influences the process of placentation, being responsible for the development of these pathologies. Being aware of this, makes us more prepared for a correct obstetrical monitoring of such pregnancies. Also, latter following of these pregnancies by Doppler evaluation of umbilical and middle cerebral arteries will influence obstetrical decisions in their attempt to decrease mortality and morbidity.
We have noticed a higher percentage of premature births in less followed patients, with fewer ultrasounds and obstetrical examinations, many of them arriving to the hospital with ruptured membranes, vaginal infection being confirmed afterwards.
All first and second trimester ultrasound markers for aneuploidy must be used to properly evaluate these high-risk pregnancies and to improve outcomes. None of them seem to be influenced by HIV infection and/or by antiretroviral treatment.
The Authors:
URSACHE Alexandra [1]
MATASARIU Roxana [1]
NEMESCU Dragos [1] [2]
BERESCU Anca [1]
TANASE Adina [1]
TIBEICA Alexandra [1]
LUCA Alexandru [2]
ONOFRIESCU Mircea [1] [2]
1 University of Medicine and Pharmacy “Grigore T. Popa”, Obstetrics & Gynecology Deptartament – Iasi, (ROMANIA)
2 Cuza Voda Obstetrics & Gynecology Hospital, 1th clinic – Iasi, (ROMANIA)
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “SOGR 2018 – 17th National Congress of the Romanian Society of Obstetrics and Gynecology & First Advanced Colposcopy Course - 2018”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “SOGR 2018 – 17th National Congress of the Romanian Society of Obstetrics and Gynecology & First Advanced Colposcopy Course - 2018”
To buy the Proceedings click here.



