Posttraumatic Stress in Physical Trauma

Abstract
An event is traumatic if it is outside the normal horizon of waiting and for all persons represents a severe stress. The syndrome with posttraumatic stress or PTSD is characterised mainly by exposing an individual to an event, workload traumatic, which exceeds its capacity to deal with the situation traumatic circumstances. Shall be specified in each of the criteria for diagnosis, that an event adverse, workload precedes PTSD.
The psychological trauma is defined by G. Fischer and P. Riedesser: “a vital experience of the discrepancy between the factors situational menacing and capabilities of the individual ownership of it, which is accompanied by the feelings of helplessness and abandon devoid of defence and which therefore result in a collapse of the duration of the understanding of himself and the world” [1].
The syndrome with posttraumatic stress (PTSD) is triggered by exposure to stimuli that the death of someone, the threat of death, serious injury to address your own person or sexual aggression. It is either of the direct experience of traumatic event, either to witness a traumatic event or bringing to the attention of the fact that a traumatic event was product to a state close to the family or close friend (such as the threat of death, the death of the violence or accident). Also, PTSD is maintained of living or repeated exposure to stimuli aversive of traumatic event by means of media, images, pictures, video, TV documentaries, and movies.
The theoretical objective: publicise the existence with posttraumatic stress in the physical trauma.
Table of Contents:
1. Introduction
2. Aetiology
3. Definition
4. Methodology
5. Final assessments
1. Introduction
Mental trauma is defined by G. Fischer and P. Riedesser as: “A vital experience of discrepancy between threatening situational factors and individual control capabilities accompanied by feelings of helplessness and abandonment that thus lead to a lasting crash of self-understanding and understanding of the world” [1].
Past traumatic experiences leave the autonomic nervous system in a state of excitation, or a traumatic reaction to stress triggers a traumatic disturbed affective state and emotional over- whelmingness. These people are more likely to experience the above-mentioned symptoms than those who were not traumatized or were previously protected [2].
Since the beginning of their existence, humans have suffered traumatic injuries through falling, fire, drowning, and interpersonal conflicts. While the lesion mechanism and the frequency of various specific injuries have changed with the time, traumas remain a very important cause of mortality and morbidity in modern society [3].
An event is traumatic if it is unexpected and for all people perceives this as severe stress. Posttraumatic Stress Disorder or PTSD is mainly characterized by exposing an individual to a catastrophic, traumatic event that exceeds his ability to deal with the traumatic situation. Each of the diagnostic criteria specifies that a catastrophic event precedes PTSD. DSM-IV-TR (APA, 2000) includes Posttraumatic Stress Disorder in the anxiety disorder. DSM-5 includes Posttraumatic
Stress Disorder (PTSD) in the category of Trauma-and-Stress-Related Disorders. This category includes disorders where a traumatic event does not precede q mental disorder.
Posttraumatic Stress Disorder (PTSD) is triggered by exposure to stimuli such as death, death threats, serious injuries, or sexual assault. This either happens by experiencing a traumatic event or witnessing a traumatic event or the realizing that a traumatic event occurred to a close family member or close friend (such as death threats, violent death or accident). PTSD is also maintained by repeated experiencing or being exposed stimuli of the traumatic event several times through media, images, pictures, videos, TV reports, and movies [4].
Disturbance causes significant stress and by consequence changing significantly the social interactions of the individual, the ability to work and other functions.
All forms of trauma, both individual (torture, rape, kidnapping, sexual and gender-based violence) and collective (war, terror) deny the human dignity and independence, violating the fundamental human rights and seriously affecting the development of the human being [5].
I think every person experience trauma at least once in their life. In recent years, society has invested heavily in trauma research and treatment methods. People are more open and more interested in the field of psycho-traumatology, as a consequence of the events in their own lives, the experiences they witnessed, the need to understand the trauma and everything that precedes it [6].
There has been an increase in the number of people who call for specialized help, who allowed themselves to feel and fight for their own well-being [7].
Once understood, the trauma can be processed, and the person can reach a level of development and functionality that is strong enough to allow personal and interpersonal relationships that represents for the individual a number of protective factors.
Through trauma therapy, individuals become aware of their own resources and activate them in order to use them as developmental support [8].
2. Aetiology
“Psychotraumatology investigates and treats a panel of relevant and pathogen-specific etiological psychological medicine” [1].
Psychotraumatology follows the psychological lesions of people to their biosphere level and explains the manifestations of trauma based on valid regulatory systems. The research maintains the broader relationship with the world as well as with humans and also discusses the specific human form of vulnerability [9].
Mental trauma is an etiological category, coming from ancient Greek, having a factitive meaning, thus being self-contained in psychology. As a cause of psychiatric trauma, three other factors have influence and must be taken into account, namely supra-socialization, when the level of education is too severe; low levels of socialization when negligence or indulgence occurs; but also, biological genetic factors, but also those acquired early [10].
Inherited factors have little influence on change. The psycho-trauma influence factor is logically the traumatic spectrum of psychiatric disorders, including posttraumatic basal stress syndrome, special psychotraumatology syndromes, dissociative disorders, and a part of the borderline disorders and pictures of somatoform disorders.
Along with a specific aetiology, traumatic disorders are a specific pathogenesis, which are the result of the trauma schema and the traumatic compensatory system [11].
Over-socialization is a factor of influence that is correlated with a rigid, excessively severe and restrictive lifestyle. The child's vitality is repressed, and the impulses and imagination systems are under the stamp of rigid printing [12]. Starting from the pathological perspective, under these conditions the classical neurotic personality develops, with a prominent identity, a vertical organization of defence, with a relatively coherent I-Self system, which can cause neurosis due to exaggerated overflow of vital impulse [13].
Low levels of socialization are the type represented by children labelled as “spoiled,” with education based on no involvement, low or unilateral normative structure. This type of education gives rise to a lack of empathy, a lack of understanding of the rules and a lack of understanding of reciprocity. These are fundamental to social relations, forming the core of the communicative principle of reality [14].
In the case of born and acquired biological factors, the focus is most ones are those acquired. From the point of view of the middle and high severity psycho-traumatic situational factors, the smallest role seems be the one of the genetic predispositions [15].
3. Definition
Mental trauma is a vital experience of discrepancy between threatening situational situations and individual capabilities that are accompanied by feelings of helplessness, abandonment and lack of protection, and thus lead to a lasting disturbance of self-understanding and the world [1].
An important element of trauma is the durable disturbance of self-understanding and the world. A trauma is relative, a relationship between the situation, threats and personal characteristics.
This “discrepancy is reached only when the type of danger exceeds the personal capabilities to overcome the danger” [16].
4. Methodology
According to Eysenck, neuroticism is related to low tolerance for stress and aversive stimuli. People who get high scores on a neurotic scale are more vulnerable to stress and reactive emotions. Negative emotional responses tend to persist for an unusually long period of time, leading to mood swings [17].
The self-administered PCL-C questionnaire reflects the traumatic symptoms and can be used on any population. This version of the questionnaire simplifies the assessment based on multiple traumas because the symptoms are not attributed to a particular event.
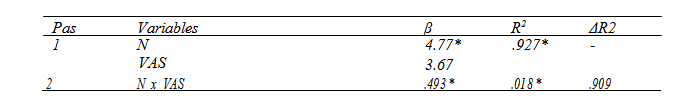
The table shows the values obtained from the analysis of moderating the relationship between Ne and PCL. Thus, in the first step, Ne and VAS explain about 93% of the variance of the PCL variable, the effect being statistically significant (R2=.927, p<.01). In the second phase the variable of the interaction between Ne and VAS was introduced in the regression model. The introduction of this variable determines an increase in the 2% explained variance, this effect being statistically significant (R2=.018, p<.01). Therefore, VAS is a moderator of the relationship between Ne and PCL.
Post-traumatic cognitions (PTCI) are a moderator in the relationship between self-perceived severity of trauma (VAS) and dissociation (DES).
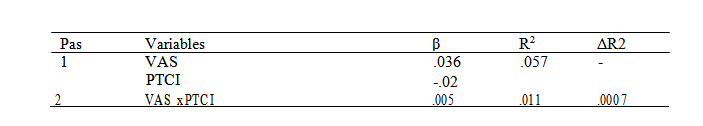
The table shows the values obtained from the moderation analysis between VAS and DES. Thus, in the first phase VAS and PTCI explain about 6% of the DES variable, the effect being insignificant statistically (R2=.057, p>.001). In the second phase the variation of the interaction between VAS and PTCI was introduced in the regression model. The introduction of this variable determines an increase of the explained variable of 0.5%, this effect being insignificant statistically (R2=.005, p>.001). In conclusion, PTCI is not a moderator of the relationship between VAS and DES.
5. Final assessments
This research is based on research into the existence of posttraumatic stress in physical trauma. An event is traumatic if it is outside the normal waiting horizon and for all people it is a severe
stress. Posttraumatic Stress Disorder is triggered by exposure to stimuli such as death, death threats, serious injuries, or sexual assault. It is either a direct experience of a traumatic event, or a witness to a traumatic event, or knowing that a traumatic event occurred to a close family member or close friend (such as the threat of death, violent death or accident). Also, Posttraumatic Stress disorder is maintained by repeatedly experiencing or being exposed to aversive stimuli of the traumatic events through media, images, pictures, videos, TV reports, and movies.
Disturbance causes clinically significant stress with consequent significant change in the individual’s social interactions, work capacity and other functions.
All forms of trauma, both individual (torture, rape, kidnapping, sexual and gender-based violence) and collective (war, terror) deny the human dignity and independence of the individual, violating the fundamental human rights and seriously affecting the development of the human being.
The results of the research have shown that people who have suffered at least one physical trauma in the last 12 months, according to DSM V, have been diagnosed as having PTSD.
Participants in the research came from distinct environments aged between 18 and 60.
Following the statistical results from the research, the following aspects were revealed regarding the presence of posttraumatic stress in physical trauma.
There was a close correlation between posttraumatic cognitions and posttraumatic symptoms, indicating that posttraumatic symptoms will increase in people with a high level of post-traumatic cognition.
Self-perceived gravity of trauma correlates with posttraumatic cognitions. The person in question tends to accentuate the self-perceived severity of trauma through thoughts, traumatic ideas, thus increasing the intensity of cognitions as well.
Post-traumatic cognitions have been closely correlated with dissociation, leading to the experimentation of higher dissociation, influenced by the increased level of cognitions.
Posttraumatic stress correlates with neuroticism. A person who has suffered a trauma is more likely to experience negative emotions and increased sensitivity, while lowering stress tolerance, with the person having frequent, mostly negative, mood swings.
Posttraumatic stress is a mental disorder manifested in various forms.
Physical traumas fall into the type of existential trauma. The intensity of these existential traumas varies according to the magnitude of the traumatic event and also the way the trauma is perceived by the person.
Physical trauma contains a wide range, such as accidents, operations, physical aggression, sexual abuse, etc.
In the research, the prevailing types of physical trauma such as accidents and operations, are the most common types of physical trauma.
Individuals who have experienced at least one physical trauma then develop post-traumatic symptoms.
The most common posttraumatic symptoms are posttraumatic cognition and dissociation. Post- traumatic cognitions amplify the perception of trauma, leading to the division of the human psyche.
Therefore, dissociation by depersonalization and derealizing, that post-traumatic symptom, has a protective role against the intrusion of psychic trauma.
The survivor of traumatic abuses and violence, physically and psychically echoed, impose on the psychologist specific ways of approaching.
The deep knowledge of the nature of its problems is not only the beginning but also the fundamental psychological intervention, by orienting the psychologist towards finding those solutions and directions of action adapted to the specifics of his problems and to the main objectives of the counselling. Francis Macnab states that every traumatized person has several types of trauma.
What is important, however, is that the central trauma that affects the most powerful person, the deepest, more disturbing psychological injury, must be identified.
The psychological repercussions encountered can be: fear, anxiety, negative image modification of the rails, sleep disorders, disorientation in space, sadness, memory disorders, psychosexual problem, apathy, isolation.
Common diagnoses were: acute stress disorder, posttraumatic stress disorder, depressive disorders.
The traumatic reaction crystallizes over time, the person concerned makes enormous efforts to accept the overwhelming situation that has passed. All this happens through a continuous game involving exchanges between the memorized elements and the defence or compensatory mechanisms that help it avoid the reappearance of panic and invasion of the senses, in other words, the re-occurrence of the traumatic event.
In conclusion, people who have had a physical trauma event of any nature during the last 12 months of life have been diagnosed through research with posttraumatic stress, unlike those who have not experienced a physical trauma in the last 12 months of life, that were not diagnosed with posttraumatic stress.
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “1st International Conference Supervision in Psychotherapy - 2018”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “1st International Conference Supervision in Psychotherapy - 2018”
To buy the Proceedings click here.



