Surgical Malpractice in Relation to Long Calls

Abstract
The working hours of surgeons have been a topic of debate in recent years. Sleep deprivation could negatively impact the cognitive function and performance, resulting in an increased risk of medical errors. This is an ethical problem for the patients, who have to achieve the best treatment possible. There are several studies that tried to find the best hours for surgeons to operate and whether sleep-deprivation affects their surgical skills.
In our study, we considered three-time intervals: the day before call, the day on-call and the day immediately after a call. We study and compared mortality and morbidity (complications, especially surgical mistakes) for the patients operated in these time-intervals.
For sleep deprived versus non-sleep deprived surgeons, we found no difference in patient mortality, nor postoperative complications.
Table of Contents:
1. Introduction
2. Matherial and method
3. Results and discussions
4. Conclusions
1. Introduction
Medical errors are a serious public health problem and a leading cause of death in most countries. In US, major medical errors reported by surgeons are strongly related to a surgeon’s degree of burnout and their mental quality of life [1].
The problems of medical errors related to fatigue and burn-out syndrome seem to be more serious for the surgical specialties and interventional procedures, even if we talk about general surgeons, or gynecologists, urology surgeons, orthopedics or endoscopists [2-7].
2. Matherial and method
Our study was prospective and descriptive, data being collected from patients’ charts, during one year of study, 2017. We took into account a heterogeneous surgery team formed by 10 senior surgeons (general surgeons, urologists and gynecologists). We considered their operations done in three distinct moments (days). These were: the day immediately before a call (cohort A), the day that the surgeons were on call (cohort B) and the day immediately following a call (cohort C), from a one-year period, 2017.
We totalize a number of 517 days on call for the 10 surgeons implied in the study, during that year. We analyzed all their patients operated by them (as principal operators) in 1551 days (the day on call, one day before and one after the call), patients’ complications and their surgery outcome.
The data led to a mean value of 4,31 call-days/surgeon/month. Considering also the day before and the day after the call, the overall time considered covered 41,9% of every surgeon’s time, including also weekend days.
We included in study all the patients operated those days: 735 patients operated on the day before the call (cohort A), 675 patients operated on call days (cohort B), and 579 operated on the day after the call (cohort C).
3. Results and discussions
The three cohorts of patients (A, B, C) were quite similar regarding the types of operations. We searched all complications encountered for the patients of the three cohorts, in follow-up periods that included the admission periods, and counting also the eventually readmissions.
The rates of complications were higher in cohort C, than in A or B, but no significantly higher. Surgical complications generally have a significant impact on intended quality of care.
Surgical patients with an initial complication are at higher risk for multiple subsequent postoperative complications [8-14].
Several studies from literature mentioned an increased rate of complication attributed to surgeons in exhausting conditions (on call or post-call).
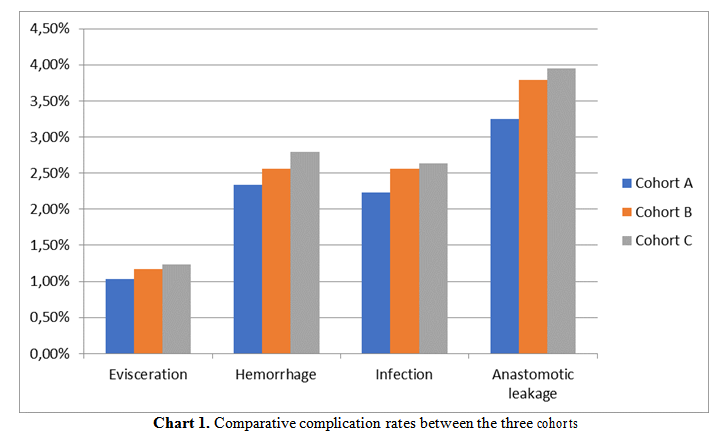
There are some categories of complications observed: eviscerations, hemorrhagic, infectious and anastomotic leakage.
The chart below reflects a comparison between the three cohorts (Chart 1).
The complication rates are a little bit higher for cohort B, compared to cohort A, and a little bit higher for cohort C, compared to B. This could be explained by principal operator exhaustion. But none of the differences has statistically significance.
4. Conclusions
The surgical complications are sometimes linked to surgeons’ fatigue. This seems to be a more subjective self-perception of surgeons than an objective fact. Surgeons tend to attribute their mistakes to burn-out syndrome, this being more acceptable for their conscience. The rates of complications do not seem to be statistically higher on call-days and the days immediately after, when exhaustion should be maximum.
The authors:
SOCEA Bogdan [1]
BOBIC Simona [1]
MOCULESCU Cezar [1]
NICA Anca Andreea [1]
DIACONU Camelia Cristina [2]
CONSTANTIN Vlad Denis [1]
BĂLEANU Vlad Dumitru [1]
TENEA COJAN Tiberiu Ştefăniţă [3]
[1] Carol Davila University of Medicine and Pharmacy, Emergency Clinical Hospital “Sf. Pantelimon”, Bucharest (ROMANIA).
[2] Carol Davila University of Medicine and Pharmacy, Internal Medicine Department, Clinical Emergency Hospital of Bucharest (ROMANIA).
[3] University of Medicine and Pharmacy of Craiova, Department of Surgery, CFR Hospital of Craiova (ROMANIA).
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “13th National Conference on Bioethics with International Participation - 2018”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “13th National Conference on Bioethics with International Participation - 2018”
To buy the Proceedings click here.



