Who’s afraid of Varicella in pregnancy?
Abstract
Introduction
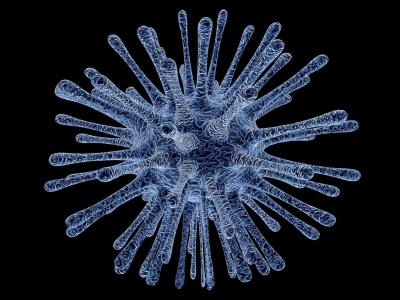
Varicella-zoster virus (VZV) is one of eight herpes viruses known to cause human infection worldwide. Varicella infection in children is generally a mild disease, while infection in adults can lead to significant morbidity and mortality. During pregnancy, varicella pneumonia can be particularly severe and maternal infection can lead to congenital abnormalities with devastating consequences [1].
If the mother acquires varicella infection during the early gestational period (weeks 8 to 20), the fetus is at risk for developing congenital varicella syndrome [2]. This syndrome is characterized by limb hypoplasia, skin lesions, neurologic abnormalities and structural eye damage.
If the mother acquires varicella immediately before or after delivery, the baby is at risk for neonatal varicella, which may present with mild rash to disseminated infection. Neonatal disease is discussed elsewhere.
Diagnosis of maternal infection with VZV is clinically based on the characteristic vesicular eruption. The incidence of varicella in pregnancy is not greater than the rest of the population.
The risk of developing congenital varicella syndrome is low 0.4%-2% [3].
Material and Method
We present three cases of primary VZV infection during pregnancy at different gestational age, whose babies did not have congenital varicella syndrome or other manifestations of VZV infection.
Common for all three cases, they were all HIV-negative (relevant as we had, previously, some cases [4]), with no other cutaneous pathologies – even related to previous radiotherapy [5] no infertility [6], previous fertility treatments [7] (and, hence, side-effects [8], [9], [10]), no previous [11], [12], [13], [14] or concomitant [15], [16], [17], [18] pathologies and no amniocenteses [19]. No alteration of the uterine contractility was seen in any of the patients.
As they, all, delivered by a cesarean section (CS), no study of partograms [20] were applicable. All CSs were performed in a classical under spinal anesthesia – with no experimental drug [21].
Table of Contents:
1. Case Reports
2. Discussion
3. Conclusions
1. Case Reports
Case I
Patient, 34 years old, 40 weeks pregnant, gravida 2, para 2, cicatricial uterus, presents at the emergency service for losing amniotic fluid and a generalized vesicular eruption that started 12 hours earlier. The patient is diagnosed with varicella (according to the infectious disease specialist’s exam). The patient gives birth by C-section to a Male fetus, with birth weight 3800g, Apgar score 8, that is handed over to the neonatology service. The newborn had a positive evolution without developing the congenital varicella syndrome.
Case II
Patient, 23 years old, pregnant, gravida 2, para 2, cicatricial uterus, presents at 16 weeks of pregnancy a generalized vesicular eruption. Following the infectious disease specialist’s exam, the patient has been diagnosed with varicella. The physician recommends pregnancy interruption and treatment with Aciclovir. The patient refuses to interrupt her pregnancy and assumes the risks to which the fetus may be subjected by exposure to VZV. At 21 weeks, the fetal morphology has been performed (without morphological anomalies visible at echography). The pregnancy presented a normal evolution until due date without any visible signs at echography of congenital varicella syndrome. The patient gives birth by C-section at 39 weeks to a Feminine fetus, with birth weight 2800g, Apgar score 9, that is handed over to the neonatology service for specialist investigations. The newborn had a positive evolution without developing the congenital varicella syndrome.
Case III
Patient, 28 years old, pregnant, gravida 1, para 1, presents at 22 weeks of pregnancy a vesicular eruption and fever. Following the infectious disease specialist’s exam, the patient has been diagnosed with varicella in the eruption period. The physician recommends treatment with Isoprinosine, locally with Aciclovir and obstetrical surveillance. At 22 weeks and one day, the fetal morphology was performed and there were no signs identified characteristic to the congenital varicella syndrome or other anomalies. The patient gives birth by C-section to a Male fetus, with birth weight 3200g, Apgar score 9, that is handed over to the neonatology service for specialist investigations. The newborn had a positive evolution without developing the congenital varicella syndrome.
2. Discussion
VZV, differently to other viruses and drugs [22], appears not to be highly teratogenic. Of course, abnormal fetuses [23] can be seen without a solid explanation. There was no effect on uterine contractility – so we could fantasize on a n on-effect on the cellular activities [24], [25], [26] or innervation [27] of the myometrium.
3. Conclusions
The risk of developing congenital varicella syndrome is very low.
Authors:
NICULESCU Costin [1]
IZVORANU Silvia [1]
PENCIU Roxana [1]
STERIU Liliana [1]
NOUR Corina [1]
POSTOLACHE Iulia [1]
[1] “Ovidius” University, Constanta County Emergency Hospital “Saint Andrew”, Constanta, (ROMANIA).
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “SOGR 2018 – 17th National Congress of the Romanian Society of Obstetrics and Gynecology & First Advanced Colposcopy Course - 2018”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “SOGR 2018 – 17th National Congress of the Romanian Society of Obstetrics and Gynecology & First Advanced Colposcopy Course - 2018”
To buy the Proceedings click here.



