Neonatal Lupus: literature review

Abstract
Neonatal systemic lupus erythematosus syndrome (NL) is a rare acquired autoimmune disorder. It refers to a wide clinical spectrum of abnormalities observed in newborn infants whose mothers have autoantibodies against Ro/SSA, La/SSB, and U1-ribonucleoprotein (U1- RNP). The major manifestations of NL are either cardiac or cutaneous findings, or both. In addition to rash and cardiac abnormalities, there may be transient hepatic, hematologic, neurologic or radiologic manifestations of NL.
Tablet of Contents:
1. Introduction
2. Epidemiology
3. Pathogenesis
4. Clinical manifestations
5. Diagnosis
5.1 Differential diagnosis
1. Introduction
Neonatal lupus (NL) is a distinct clinical entity characterized by passive transplacental passage of maternal anti-Ro/SSA (Sjögren syndrome type A antigen) and/or anti-La/SSB (Sjögren syndrome type B antigen) and U1-ribonucleoprotein (U1-RNP) antibodies that affect neonatal organs, resulting in fetal and neonatal disease. [1] Sjogren’s syndrome is an autoimmune disorder characterized by lymphocytic infiltrates of exocrine glands resulting in glandular dysfunction (preferentially salivary and lacrimal glands), that affects mainly women. It can be classified into primary Sjogren’s syndrome which occurs in the absence of other autoimmune diseases and secondary Sjogren’s syndrome which presents along with other autoimmune diseases such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE). [2]
2. Epidemiology
NL is responsible for over 90% of all cases of congenital complete heart block (CBH) in the absence of structural defects diagnosed in utero or in the neonatal period [3].
Approximately 2% of newborns with mothers who have antibodies to Ro/SSA and/or La/SSB develop cardiac manifestations at the initial diagnosis or later as opposed to newborns from mothers with U1-RNP who usually develop only cutaneous manifestations. [2] The risk increases to 18%, if a previous child had complete heart block or cutaneous NL and the risk of recurrence of rash is approximately 30 percent. [4], [5] These specific autoantibodies (Ro/SSA, La/SSB) are associated with NL independent of maternal disease and almost half of mothers with these autoantibodies who do not have other evidence of autoimmune disease at the time of the baby’s birth develop autoimmune disease later. [6], [1], [2]
3. Pathogenesis
NL is presumed to result from the passive transplacental passage, but the pathogenesis probably requires more than the presence of these antibodies in the fetal circulation since it is relatively rare, even when high titers of these antibodies are present. Thus, a high titer alone is not enough to result in CHB. [7] In addition, discordance of disease, especially of heart block, in monozygotic twins has been reported. [8]
Injury to the fetal heart most often occurs during the 18th-24th weeks of gestation and is presumed to be dependent on IgG transport by neonatal Fc receptor of maternal IgG autoantibodies. Heart block results from binding of anti-Ro/SSA and/or anti-La/SSB antibodies to fetal cardiac cells that have undergone physiologic apoptosis during remodeling, leading to autoimmune injury and secondary fibrosis of the atrioventricular (AV) node and its surrounding tissue. [1], [3]
Autoantibodies may also act by inhibiting calcium currents mediated by cardiac L and T type calcium channels. [9] L type channels are crucial to action potential propagation and conduction in the AV and sinoatrial (SA) nodes, while the functional role of the T type channel in the AV node is not completely understood. [1], [2] The fact that heart block develops in only a minority of subsequent pregnancies, despite the persistence of maternal anti-Ro/SSA and/or anti-La/SSB antibodies, strongly suggests that fetal factors are important determinants of risk. Some studies suggest that fetal susceptibility to heart block may be influenced by specific human leukocyte antigen (HLA) alleles [3], which are associated with skin disease significantly greater than the association found in patients with discoid lupus erythematosus. Maternal-fetal micro-chimerism may contribute to CHB in NL and thus, semi- allogenic maternal cells could be the target of an immune response. [2]
4. Clinical manifestations
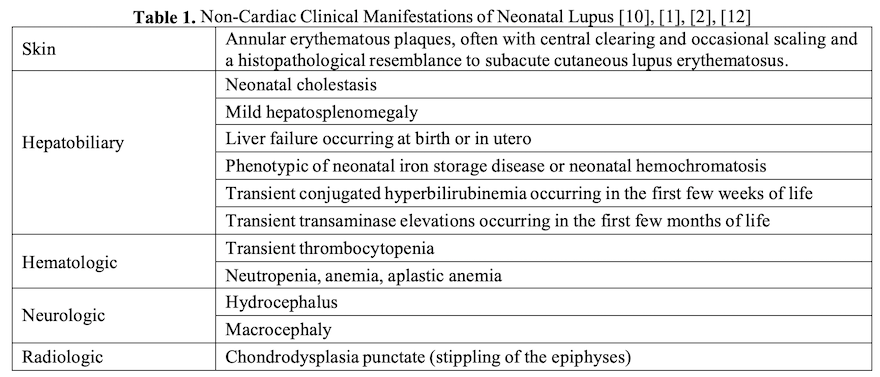
A newborn can have either cardiac or cutaneous findings or both as the major manifestations of NL and other non-cardiac manifestations may also be present. (table 1)
The rash can be present at delivery in some cases or may develop after exposure to ultraviolet (UV) light, which induces or exacerbates the rash. [10] It can appear up to approximately four months of age and almost always resolves by six to eight months of age because the half-life of immunoglobulin G (IgG) antibodies is approximately 21 to 25 days. [1], [2]
It usually comprises erythematous annular lesions or arcuate macules with slight central atrophy and raised active margins that are located primarily on the scalp and periorbital area often resulting in a raccoon-eye appearance, or on other parts of the body such as the palms and soles or the diaper area. [10] Because NL skin lesions that appear postnatally are independent of breastfeeding [11] it is not contraindicated for mothers with anti-Ro/SSA and/or anti-La/SSB antibodies to breastfeed.
The more advanced forms of heart block present as fetal bradycardia except first-degree block. The most serious manifestation of NL is third-degree or complete heart block where there is complete dissociation of atrial and ventricular rates because there is no atrioventricular (AV) conduction. The atrial rate is usually normal, and the ventricular rate is between 50 and 80 beats per minute (bpm) but can be lower or higher. [3] Pathological findings include fibrosis/calcification of the atrioventricular (AV) node, sinoatrial (SA) node and bundle of His, endocardial fibroelastosis (EFE), papillary muscle fibrosis, valvular disease, calcification of the atrial septum and mononuclear pancarditis. Fibrosis of the AV node/distal conduction system is the most characteristic histopathological finding. [13] EFE can occur in addition to conduction defects [2] and has also been reported in the absence of a conduction defect in infants exposed to maternal anti-Ro/SSA and anti-La/SSB antibodies. [14]
Although autoantibody-mediated heart block in NL is typically associated with a structurally normal heart, other congenital structural cardiac anomalies are observed in association with NL and include persistent patent ductus arteriosus, patent foramen ovale, pulmonic stenosis, pulmonary valvular dysplasia, fusion of chordae tendineae of the tricuspid valve, ostium secundum type atrial septal defects as well as hydrops fetalis. [13], [1], [3]
5. Diagnosis
The diagnosis of NL is made when the following are both present:
1. The mother has anti-Ro/SSA (Sjögren syndrome type A antigen), anti-La/SSB (Sjögren syndrome type B antigen) or anti-ribonucleoprotein (RNP) antibodies.
2. The fetus or newborn develops heart block or the typical rash or hepatic or hematologic manifestations in the absence of another explanation.
5.1 Differential diagnosis
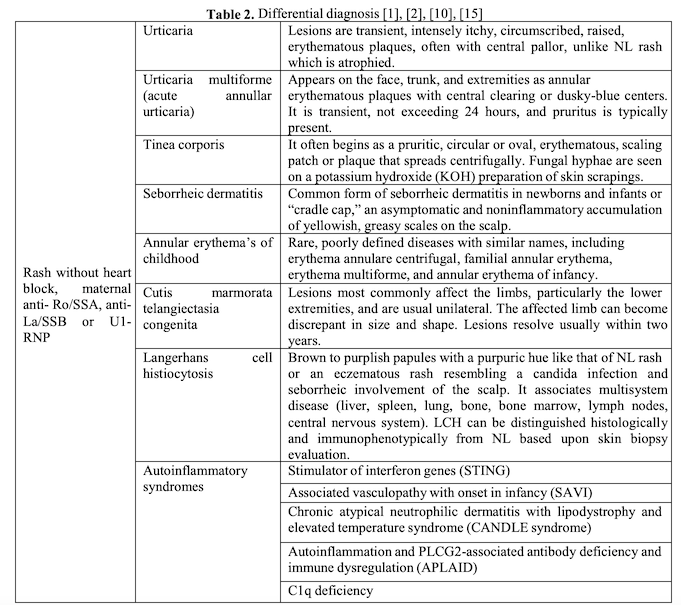
The differential diagnosis of NL cutaneous manifestations includes various rashes seen in the newborn period. These rashes are not associated with congenital heart block (CHB) or with Sjögren syndrome type A or B antigen, or anti-ribonucleoprotein (RNP) antibodies. (Table 2)
6. Postnatal management
Postnatal management primarily depends upon what degree of heart block, if any, was noted in utero and what the findings are on initial neonatal electrocardiogram (ECG) which should be performed on all neonates born to mothers with anti-Ro/SSA and/or anti-La/SSB antibodies, even in the absence of any in utero cardiac abnormalities. Furthermore, a pediatric cardiology consult should be obtained if fetal monitoring has detected any degree of heart block in utero (including PR intervals >3 standard deviations [SD] or 150 msec, or second- degree block that reversed) and/or if the neonatal ECG is abnormal. If first- or second-degree heart block is identified after birth, careful observation of these infants is necessary as there is a risk of postnatal progression to a higher-degree block, including complete heart block. [16], [4], [1]
Infants with second-degree block in utero that reverted to normal sinus rhythm (NSR) and that have NSR at birth should be evaluated within the first three months of life as they are still at risk of developing third-degree heart block. [16] In the case of complete heart block insertion of a cardiac pacemaker is required, especially if the heart rate at delivery is less than 55 beats per minute (bpm). The prognosis following pacemaker implantation is excellent for most children, although development of heart failure may occur. If NL manifest as noncardiac involvement after birth with no evidence of heart block of any degree at birth (exam and ECG) it unlikely that late de novo development of complete heart block develops. [17] Although rare, children who have had NL may be at increased risk of developing an autoimmune and/or rheumatic disease, with oligoarticular and polyarticular juvenile idiopathic arthritis, psoriasis, thyroid disease, iritis, type 1 diabetes mellitus, and nephrotic syndrome. [18]
The rash does not usually require treatment, but topic corticosteroids may hasten the resolution of the lesions and sun protection is advised, including avoidance of direct sunlight and fluorescent light. [10][1][2]
The authors:
RADULESCU Luiza [1] [2]
NASTASE Leonard [1] [2]
RADULESCU Iulian Mihai [3]
MOHORA Ramona [1] [2]
STOICESCU Silvia-Maria [1] [2]
[1] University of Medicine and Pharmacy “Carol Davila” (ROMANIA).
[2] National Institute of Mother and Child Health (ROMANIA).
[3] Bucharest University Emergency Hospital (ROMANIA).
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “4th Congress of the Romanian Society for Minimal Invasive Surgery in Ginecology – Annual Days of the National Institute for Mother and Child Health Alessandrescu-Rusescu - 2018”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “4th Congress of the Romanian Society for Minimal Invasive Surgery in Ginecology – Annual Days of the National Institute for Mother and Child Health Alessandrescu-Rusescu - 2018”
To buy the Proceedings click here.



