Surgical Treatment in Endometriosis
Abstract
Endometriosis is a complex disease with a wide spectrum of symptoms. Women with endometriosis classically present during their reproductive years with pelvic pain (including dysmenorrhea and dyspareunia), infertility, or an ovarian mass. It can be either asymptomatic, or, in cases of extensive disease, it is characterized by debilitating pain, bowel and bladder dysfunction, abnormal uterine bleeding, low back pain, or chronic fatigue, although these symptoms are less common. The management of endometriosis is complex and it can be either medical or surgical. Surgery also represents a good diagnosis tool as it offers the chance of histological tissue examination and it in cases of laparoscopic route it is an excellent opportunity for staging. The aim of this paper is to underline the importance of surgery in endometriosis management.
Table of Contents:
1. Introduction
2. Surgery in endometriosis
3. Conclusion
1. Introduction
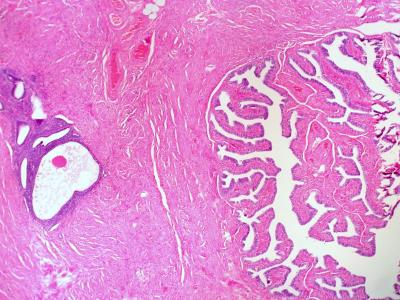
Endometriosis is a complex disease and its incidence becomes more and more frequent. It represents an abnormal gynecological condition characterized by the presence of endometrial glands and stroma outside the uterus. It is estrogen dependent and it usually affects women during their reproductive years. This ectopic tissue can be present anywhere in the body, including bowel, diaphragm or pleural cavity, but it is more frequent in pelvis. The disease can be asymptomatic, or the symptoms can vary from various types of pain to unexplained infertility.
The American Society for Reproductive Medicine Practice Committee consider that “endometriosis should be viewed as a chronic disease that requires a lifelong management plan with the goal of maximizing the use of medical treatment and avoiding repeated surgical procedures” (1).
The treatment should depend on clinical presentation (infertility, pain, ovarian mass), extension and location of disease, age, reproductive desires, symptom severity or contraindications or side effects of medication. Thus, the treatment can be medical or surgical.
Before any treatment, every woman should have a detailed history and evaluation and other causes of pelvic pain should be excluded.
Chronic pelvic pain is described as a non-cyclic pain in a nonpregnant woman, unrelated to menses, that lasts for a period of at least 3-6 months, it is severe enough to cause functional incapacity and to require special treatment (2-4) and it is usually the main target of medical management in endometriosis.
Medical management is represented by various classes of drugs that can modulate the intensity of pain. Non-nonsteroidal anti-inflammatory drugs, combined estrogen-progestin contraceptive pills, gonadotropin-releasing hormone agonists or antagonists, danazol or aromatase inhibitors are several options for dealing with the disease. The treatment choice is based on the symptoms severity, side effects and contraindications, availability, contraceptive needs and patient choice (5, 6).
There are no standard recommendations for one treatment over another. The advantages of medical therapy are the avoidance of damaging pelvic organs during surgery, the avoidance of postoperative adhesion formation and the capacity of treatment of the implants that are not visualized during investigations or surgery. Some of the disadvantages may be the side effects of the medications, the high recurrence rate in case of discontinuation of treatment, no effect on endometriomas or existing adhesions and no effect on infertility.
2. Surgery in endometriosis
Surgical treatment involves both diagnosing the location and extent of endometrial lesions and treating the lesions with some form of destructive therapy.
The major advantage of surgery is that it provides tissue for histologic examinations and a clear diagnosis. The indications for surgery are represented by the persistence of pain despite medical therapy, the refusal or contraindications to medical therapy, obstruction of the bowel or urinary tract or exclusion of malignancy in an adnexal mass (1, 5). Usually there is a high suspicion index of endometriosis after several investigations and the surgery just confirm the diagnosis, but there are cases when ultrasound is quite ambiguous and surgery is needed for exclusion of malignancy (7).
Surgery should be avoided in women with incomplete evaluation of pelvic pain, women with persistent pain after repeated surgeries or women near menopause. Usually the symptoms resolve with menopause and thus, those women who are in perimenopause may tolerate the pain in order to avoid surgery. The decision for surgery in these women depends upon the balance of the quality of life with or without surgery. Some disadvantages of surgery are the risk of adhesion formations, reduction of ovarian reserve or the risk of organs injury (bladder or bowel most frequent). Despite the benefits, there are some disadvantages of conservative treatment. The recurrence of symptoms is higher than in women with definitive surgery and the rate of reintervention increase over time and the expected benefit is operator-dependent (8-10).
Surgical treatment in endometriosis can be either conservative or definitive. The conservative types are the first line treatment for women who desire a child. It consists in excision or ablation of the endometriomas or other lesions, preserving the uterus and as mush ovarian tissue as possible (1). In preserves fertility and hormone production, is less invasive and has less complications as definitive surgery.
Definitive surgery is represented by hysterectomy, with or without oophorectomy. It is recommended to women with severe and persistent symptoms despite other therapies and to women who completed childbearing (1).
Hysterectomy is recommended for women without any plans for future fertility, with debilitating symptoms who have failed the medical therapy and at least one conservative procedures. It is also recommended for women with additional indications for hysterectomy like persistent uterine bleeding, symptomatic fibroids or prolapse). Although the recurrence rate of symptoms is lower in women with hysterectomy compared to conservative treatment, the main disadvantage of the procedure is the loss of the reproductive ability and the risk of more complications.
Hysterectomy alone, without oophorectomy, is performed for women who desire pain control and preservation of ovarian hormonal function. The hormonal function is maintained longer in women with conservative therapy compared to those treated with hysterectomy without bilateral salpingo – oophorectomy (11-13).
Oophorectomy is mainly recommended for women with extensive adnexal disease. It is usually performed in women older than 40 years. In cases where the risk of premature menopause is lower than the risk of recurrence, oophorectomy is also indicated. Because endometriosis is estrogen dependent, removal of the ovaries may reduce the symptoms related both to pelvic or distant disease. The major disadvantage is premature menopause and potential long term health effects, like the increased risk of cardiovascular disease, osteoporosis, neurologic disease or psychiatric illness (14-16).
The technical approach is via laparoscopy or laparotomy. They are both equally effective in treating the chronic pain related to endometriosis (5). Laparoscopy is less invasive and it is associated with better cosmetic results, less pain, shorter recovery period and shorter hospitalization (5, 17, 18). One major disadvantage is the dependence of the operator skills and that special training is needed for laparoscopic procedures. Almost all types of procedures can be performed via laparoscopy, independent of the severity of the disease. In offers the possibility of visualization of the whole peritoneal cavity thus permitting a better staging of the disease. In cases of infertility and chronic pelvic pain associated with severe endometriosis both laparoscopy and laparotomy seem equally effective. However, some studies suggest that a higher pregnancy rate and lower dyspareunia recurrence rate after surgery for severe endometriosis were observed in women treated with laparotomy compared with laparoscopy (17).
Laparotomy is preferred in cases with extensive disease like adhesions or invasive endometriosis located near uterine arteries, ureter, bladder or bowel. For trained surgeons, robotic surgery may be an option for surgical therapy in endometriosis. There are few studies that compare the results and complications between the two mini-invasive procedures, but in general there were no differences in mean operative time, complication rates or rates of conversion to laparotomy between the two procedures (19).
The importance of surgical therapy is the possibility of exploration the peritoneal cavity to classify the severity of the disease. There are some classification systems with poor correlation with pregnancy outcome or pain, but the progression of the disease between several procedures can be noted (20, 21).
The destruction of the endometriotic lesions is performed by ablation or excision. Ablation eradicates the lesions by laser vaporization, electrosurgical fulguration or coagulation.
Almost 70% of women with endometriosis develop extensive intraperitoneal adhesive disease (22). Red lesions are associated with more adhesions than black, white, and clear lesions. Often, adhesions appear as a part of postoperative healing and in some cases may exacerbate pain or infertility, thus surgical resection is not always effective in reducing pain (23).
In some cases, the extensive pelvic adhesions may limit the mobility and visualization of the pelvic organs, condition that cannot always be anticipated prior to surgery, situation called frozen pelvis. The operative goal in these cases is to establish the normal anatomy.
Presacral neurectomy may be indicated in cases of refractory disease, but it can be associated with constipation of urinary disfunction (24).
3. Conclusion
Surgery in endometriosis represents a valuable tool both in diagnosis and treatment of the disease. The various procedures, either conservative or definitive, have specific indications.
The conservative procedures maintain fertility and offer the women a chance for completing childbearing. The radical procedures are used in cases of recurrent disease despite aggressive medical treatment or in women to whom childbearing is not an option anymore.
Authors:
VINTEA Alexandra [1],[2],
DRAGOMIR Ramona [2],
FÎRȚĂ Anca Roxana [2],
BĂNCEANU Gabriel [1]
[1] “Carol Davila” University of Medicine and Pharmacy, Bucharest, (ROMANIA).
[2] “Alessandrescu-Rusescu” National Institute for Mother and Child Health, Polizu Department, Bucharest, (ROMANIA).
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “4th National Congress of HPV - 1st Congress of the Society of Endometriosis and East-European Infertility - 2018”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “4th National Congress of HPV - 1st Congress of the Society of Endometriosis and East-European Infertility - 2018”
To buy the Proceedings click here.



