The impact of treating chronic rhinosinusitis in sleep disorders

Abstract
Chronic rhinosinusitis is a common disease of the paranasal sinuses affecting aproximatly 16% of the world population. Studies have linked chronic rhinosinusitis to poor sleep quality and even sleep disorders with approximately three quarters of of patients suffering from chronic rhinusitis complaining of poor sleep quality. Chronic rhinosinusitis causes a marked decline in quality of life and the association of various sleep disorders further decreases the quality of life being linked to daytime sleepiness, impaired cognitive function and even depression. The main risk factors for sleep disorders in chronic rhinosinusitis are smoking, obesity and in some cases allergic rhinitis. Altough there is a high prevalence of sleep disorders in chronic rhinosinusitis there are few studies that have investigated the mechanism implicated in the association of the two.
Methods
We present the results of 20 patients who were admitted in our clinic for surgical treatment of chronic rhinosinusitis that also complained of poor sleep quality. They were asked to complete a VAS score relating their sleep quality before and after the surgery. They were also asked to quantify their daytime sleepiness before and after the surgery.
Results
The results showed improvements in sleep quality and daytime sleepiness in the majority of cases indicating that there is a possible connection between chronic rhinosinusitis and sleep disorders and that treating chronic rhinosinusitis improves both quality of life and the quality of sleep.
Table of Contents:
1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
1. Introduction
Chronic rhinosinusitis is one if the most common affection for which patients seek medical advice. It affects approximately 16% of adults interfering with the drainage and causes mucus buildup. It can be caused by infections (Staphylococcus aureus, Haemophilus influenza, Moraxella catarhalis) [1] or anatomical structures like a deviated septum [2]. In some cases, even periodontal disease can be a risk factor for developing chronic rhinosinusitis [3].
The symptoms are nasal obstruction that causes difficulty breathing, reduced sense of smell, nasal discharge and sometimes pain or tenderness in the area of the paranasal sinuses [4, 5]. Among other symptoms we can find ear pain, sore throat, coughing and sometimes bad breath. Some patients also complain of poor sleep quality or even sleep disorders. Studies have shown patients with chronic rhinosinusitis suffer from sleep disorders at a significantly higher proportion then patients without chronic rhinosinusitis.
Although little is known about the mechanism of sleep disorders in patients with chronic rhinsinusitis, poor sleep appears to be one of the main reasons that convinces patients to seek medical treatment. It appears that the mechanism is multifactorial like facial pain, nasal obstruction or constant rhinoreea. In some cases, chronic rhinosinusitis can aggravate symptoms from previously documented sleep disorders like sleep apnea. Chronic rhinosinusitis affects the quality of life and it is associated with high costs worldwide [6] from lost productivity and the association with poor sleep quality can lead to depression and daytime sleepiness.
2. Methods
We present a study that was performed in our clinic that included 20 patients diagnosed with chronic rhinosinusitis. Patients complained of nasal obstruction and loss of smell. They also told about daytime sleepiness and fatigue and accused poor sleep quality. The patients were admitted in our clinic for the surgical treatment of chronic rhinosinusitis after medical treatment had little effect in relieving symptoms. All the patients had undergone a computer tomography before surgery. All patients signed an informed consent about taking part in our study and were asked to complete a questionnaire about daytime sleepiness and a VAS questionnaire about sleep quality. A complete medical history was made for each patient taking in account various risk factors and body mass index.
Patients underwent a pre-anaesthesia examination. As for all new admissions in the ENT clinic, all patients had nasal swabs collected from their nostrils as part of MRSA screening, a frequent opportunistic pathogen found that can be found in hospital environments [7] All patients underwent functional endosocopic sinus surgery under general anaesthesia and were discharged without any complications. Patient were asked to come for a follow up examination one week post surgical treatment and again after one month and 3 months.
They were asked to complete the same questionnaires again at one and three months after the surgical procedure. Only patients who did not lose weight or changed their pre-surgical lifestyle were considered so that the changes in score are not due to those changes. The VAS scale was comprised of 10 levels that patients used to assess their subjective impression about sleep quality. The daytime sleepiness questionnaire is based on the Epworth scale suited for our patients.
3. Results
Only patients that returned at the follow up controls and completed the questionnaires were considered. For the final analysis only, patients that did not change their lifestyles (body mass, smoking) were considered so that no other variable change would change the results.
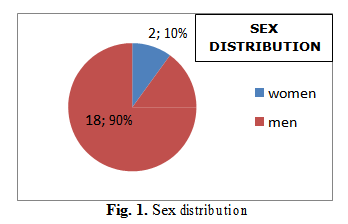
In our study out of the 20 patients 18(90%) were male and 2(10%) were females as shown in Fig 1. The mean age of the group was 52.54 years old and 90% of the patients were smokers.
None of the patients underwent previous sinus surgery and none of them used medication with sedative effects.
All patients underwent endoscopic sinus surgery under general anaesthesia with no postsurgical complications.
The daytime sleepiness median score before surgery was 12.45 in our group of patients.
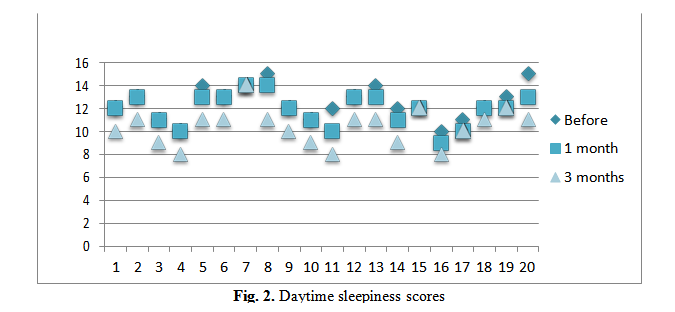
At the one month follow up patients completed the daytime sleepiness scale and the median result was 11.9 A slight improvement given that the majority of patients said that the first week postsurgical treatment their symptoms worsened.
At three months after surgery the patients score median was 10.35 a 17.2% improvement form the score median before surgery.
Vas Score
Patients were also asked to complete a VAS to mark their impression of sleep quality. Tha VAS ranged from 0-10 where 10 being the extremely poor sleep quality and 0 a high-quality sleep.
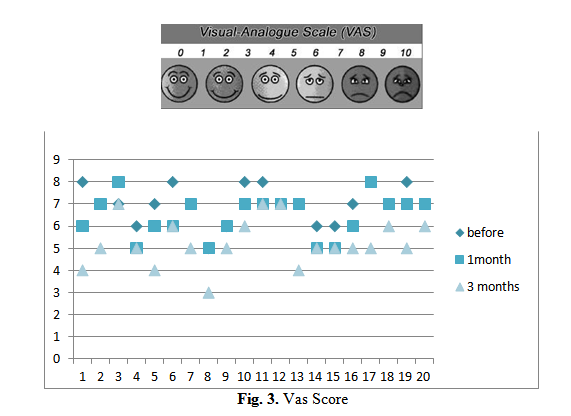
The median vas score before surgery was 7. The median score at 1 month after surgery was
6.45 and 5.25 at3 months after surgery. Again, an improvement in the scores compared to the result before surgery.
4. Discussion
The result showed that there is slight improvement in both daytime sleepiness and in sleep quality after surgical treatment of chronic rhinosinusitis. Although there are some limitations of this study in the sense that the measurements were subjective and depended on the patient’s ability to objectify their sleep quality and daytime sleepiness there seems to be a connection between chronic rhinosinusitis and sleep disorders.
Although little is understood regarding the way chronic rhinosinusitis produces sleep dysfunction many hypotheses exist in present.
Mahdavinia states that patients that have chronic rhinosinusitis are affected by sleep disorders (60-75%) in a larger proportion than the general population. Sleep disorders affect quality of life and can lead depressions and depraved cognitive function as well as important affections like hypertension and cardiac disease. [8]
Quinn states that following treatment of chronic rhinsinusitis there is a subjective improvement of sleep quality but further studies that explain the physiology of the association between chronic rhinosinusitis and sleep disorders are needed. [9]
A study made by Jiang on a group of 139 patients with chronic rhinosinusitis showed that 38% of the patients complained of daytime sleepiness related to the onset of nasal obstruction.
Obstructive sleep apnea was diagnosed in 64% of these patients. [10]
Patients with obstructive sleep apnea declare an improvement in subjective sleep quality after an endoscopic sinus surgery for chronic rhinosinusitis. [11]
Bengtsson et al., reported that in the study conducted out of 26647 subjects 8.4% had chronic rhinosinusitis and reported sleep problems were 50-90% more common among subjects with chronic rhinosinusitis compared to those without or general population. [12]
5. Conclusions
Chronic rhinosinusitis is a common disease with high economic implications that affects the quality of life. Its association with sleep disorders further affects the quality of life and can lead to important comorbidities like cardiac disease, hypertension, failure to meet social obligations and depression. Although the mechanism in which chronic rhinosinusitis can lead to sleep disorders in partially unknown more and more studies have linked it with sleep disorders like sleep apnea.
Risk factors like smoking, obesity, anatomical structures like a deviated septum are usually found in both diseases. It is important the more studies are made about the correlation between chronic rhinosinusitis and sleep disorders.
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “National ENT, Head and Neck Surgery Conference - 2018”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “National ENT, Head and Neck Surgery Conference - 2018”
To buy the Proceedings click here.
Gli autori di questo articolo:



