Male sexual dysfunction in diabetes patients. Diagnostic and therapeutic management options

Abstract
Diabetes mellitus (DM) is the cause of multiple medical and psychological complications. The increase in DM prevalence, both Type 1 and Type 2, and its complications, also entails an increase in the incidence of sexual dysfunction in these patients, this being considered one of the early complications in this category of patients. Male Sexual Dysfunction (DSM) is much better investigated and documented today, and medical treatment is complemented by lifestyle optimisation, psychological counselling and, last but not least, good DM control.
Table of Contents:
1. Introduction
2. Materials and Methods
3. Results and Discussions
4. Conclusions
1. Introduction
Diabetes mellitus (DM) is one of the most common chronic diseases and is a real public health problem. The number of people suffering from DM is on the increase due to urbanisation, increasing the prevalence of obesity and reducing physical activity on the other hand, due to the rise in life expectancy, the emergence of modern and sophisticated investigations as well as new therapies in the field.DM is the cause of multiple complications, both medical and psychological.
The increase in DM prevalence and its complications also entails an increase in the incidence of sexual dysfunction in these patients. Numerous studies have shown that DM patients are at increased risk of developing sexual dysfunction earlier than 6-10 years compared to non-diabetic patients. This is due to poor control of DM, its age, but also to the presence of its complications [1]. Sexual dysfunction may be the first sign of deterioration in vascular status in patients with DM [2, 3].
2. Materials and Methods
We conducted a review of the literature by looking into the MEDLINE database of the most representative articles published so far. More than 20 articles were selected from the research, using the search by keywords: diabetes; diabetic erectile dysfunction; diabetic neuropathy, endothelial dysfunction; phosphodiesterase inhibitors and intracavernous injection.
3. Results and Discussions
Diabetes mellitus (DM) is responsible for lesions of the somatic and autonomic peripheral nervous system, urinary tract injuries as well as psychological changes. Vegetative diabetic neuropathy affects almost all organs, especially: heart, kidney, urinary bladder, gastrointestinal apparatus, pupil but also the reproductive system. Sexual deficiencies are common problems for diabetic patients and are primarily related to the degree of glycemic control and the duration of diabetes. Sexual and urological complications are the cause of the damage to both nerves and small blood vessels.
It is estimated that 30 million male Americans develop along the evolution of DM erectile dysfunction (ED). Male impotence can develop at any age, but usually the most affected are senior men. A recent study of 1300 patients showed that 52% of the patients in the suds had different degrees of erectile dysfunction and their age was between 40 and 70 years. Over 50% of the 10 million men diagnosed with type 2 diabetes have various degrees of sexual impairment. In patients with well-controlled DM, the impotence rate is lower, while patients with poorly controlled DM between 50-70% of men with sexual dysfunction [4, 5].
Nowadays, the prevalence in patients with DM is 28%, probably much underestimated, and is present in subjects aged 40-70 years, compared with the incidence in non-diabetic subjects, where the values are about 9.6%. The age at which ED is established in patients with DM is lower than in non-diabetic patients, with a prevalence of 1-10% in 30-year-old men reaching
20-40% in those aged 60-69 years. Of ED patients, nearly 40% are diabetics, of whom more than a quarter were not diagnosed with DM, in other words, the ED diagnosis was almost concomitant with the DM diagnosis [6]. A recent study showed that at least 11.5% of patients with ED had undiagnosed diabetes [7]. The prevalence of ED in patients with Type 1 DM and Type 2 DM is equal. ED is more common in diabetic patients with neuropathy [5-7].
DSM is much easier to diagnose and is the most well-studied pathology of sexual dysfunction.
DSM is also referred to as erectile dysfunction (ED) and represents the inability to obtain and maintain a penile erection sufficient for satisfactory sexual intercourse [8, 9].
From an etiopathogenic point of view, ED is a disease with multiple trigger factors. Not always cause-effect association is well established and documented. ED can be various, from psychogenic erectile dysfunction, neurological disorders (parasympathetic vegetative system) endocrine, veno-occlusive incompetence, iatrogenic causes, drugs to cause infectious causes (balanitis, prostatitis).
In patients with ED and DM, the factors involved in ED are more specific as age, duration of DM, glycemic control level by evaluation of glycosylated hemoglobin (HbA1C%), presence of micro- and macrovascular complications, especially neuropathy and vascular damage, dyslipidemia, smoking, alcohol consumption, treatment followed for both DM and its complications, disorders of androgen secretion, as well as alteration of endothelial function and contractility of the cavernous muscle. Several recent studies have also shown a direct link between vitamin 25 (OH) D and ED deficiency.
On the other hand, in this category of patients, the psycho-emotional disorders have an important role in triggering the pathology [10, 11].
The ED classification, according to the International Index of Erectile Function (IIEF-5) Questionnaire, is divided into 4 stages, depending on the scores that this questionnaire records: score 22-25 points = no ED, 17-21 points = ED mild, 12-16 points = moderate ED, 8-11 = Moderately severe ED, 5-7 points = severe. The chest is validated and is a very lasting tool in ED evaluation along with clinical and laboratory investigations [12, 13].
From a pathophysiological point of view, penile erection depends on the increase in blood flow in the cavernous body, which in turn depends on the infusion pressure, the relaxation of the arterioles that irrigate these bodies and the relaxation of the cavernous muscle. The atheromatous bone is frequently associated with DM by 40% more than non-diabetics. The atheromatous attenuation of the internal shingles and the internal iliac artery may explain the poor erection. In diabetic patients nocturnal penile tumescence (TPN) is much reduced [14] and the explanation may be related to neuropathic affection but also the primary area of dysfunction is at the level of NO synthesis and release, both from the neural and endothelial sources, but not from the intracellular level of the cavernous muscle [15].
Endothelial cells form a permissive layer that regulates the flow of nutrients and the action of bioactive circulating molecules in the blood on the underlying tissue, mainly vascular smooth muscle. This is achieved by a series of receptors attached to the membrane and junctional proteins. The primary marker of dysfunction endothelial cells in diabetics is the presence of microalbuminuria, thus indicating the presence of renal microangiopathy. Therefore, the low activity of NOSe, the inactivity of NO barely released and the growth of advanced glycation end products (AGES) are the mechanisms involved in ED. The three phases of erection (excluding detumescent phase) are characterised by different clinically established parameters (Table 1).
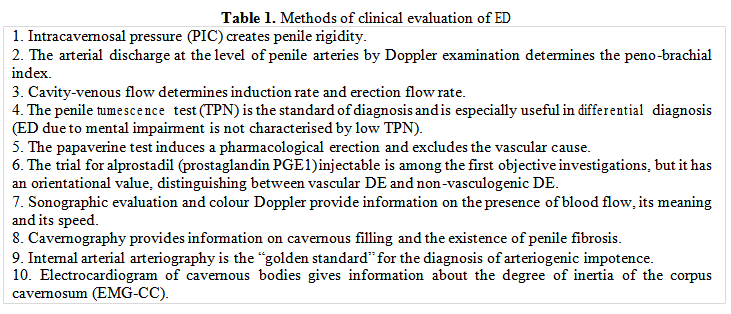
The clinical diagnosis of ED is not the first easy to translate. A detailed history, including a personal account, the duration of diabetes, its degree of control (HbA1c%), the presence of hypoglycemia, the presence of complications, the pharmacological treatment of DM/complications, the compliance to treatment and diet, the family/comorbidities, alcohol/alcohol status, surgery history, sleep disturbances can often be present and can mask an ED. In this context, the ED history should be detailed and include information on the history of sexual function, reproductive history, the age of dysfunction, the way of installation (sudden/slow), aspects of intimate life: the couple's relationship, traumas, abuses. The general and specific abstracts must most often be doubled by the physical and biochemical examination, general and specialist investigations (urology -andrology, diabetes) as well as a psychological evaluation (see also Table 1).
Once the ED has been established, and its degree can be made a treatment plan. Currently, therapeutical options are multiple and include, on the one hand, DM treatment and on the other hand ED treatment and action on risk factors: cessation of smoking, limiting alcohol consumption and regular exercise. The choice of treatment will be made by a multidisciplinary team including the urologist, diabetologist, psychologist/psychiatrist, sexologist and andrologist [16]. Most of the time, the improved chronically imbalanced glycemic imbalance does not lead (HbA1c), and future complications have also found improvement in DE.
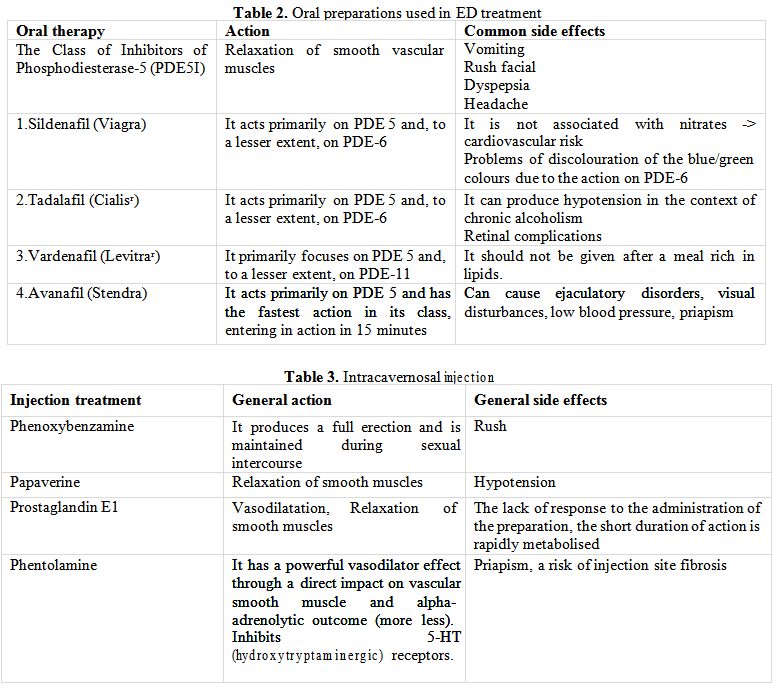
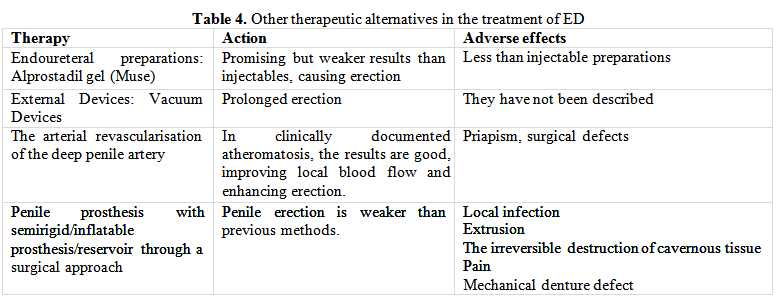
Antidiabetic medication can be criminalised for the onset or deterioration of ED only if, within two weeks of therapy administration, there is a sudden decline in ED. Elimination of risk factors, psychological/sexual counselling, testosterone therapy - initiated only in the context of hypogonadism clinically proven by hormone dosing (testosterone, SHBG) along with oral and injectable preparations recommended in ED complete the therapeutic management (Tables 2, 3, 4).
Recent results have shown that administration of L-arginine or L--citrulline improves erectile function. These amino acids have the potential to increase nitric oxide and indirectly increase penile blood flow. This aspect is even more important in people with DM where the level of nitric oxide is low [17]. And the administration of vitamin D has a beneficial effect in patients with ED, diabetes and 25 (OH) vitamin D deficiency [18, 19].
4. Conclusions
ED is today better diagnosed, investigated and treated. The most important step is to correctly diagnose the diagnosis, more precisely if the ED is psychogenic or organic [20]. It is a real psychological problem when installing the first Symptoms of ED, but the collaboration between specialists of diabetes, urologists, gynaecologists and psychologists makes these pathologies much better today, increasing the quality of life of patients with DM. The treatment must be phased out, as proposed above, and interventional cardiology procedures, as well as revascularisation procedures, can bring real benefits to ED patients.
Contributo selezionato da Filodiritto tra quelli pubblicati nei Proceedings “International Conference on Translational and Integrative Medicine - 2018”
Per acquistare i Proceedings clicca qui.
Contribution selected by Filodiritto among those published in the Proceedings “International Conference on Translational and Integrative Medicine - 2018”
To buy the Proceedings click here.



